Anecdotal evidence suggests that people are using Cannabidiol (CBD), the non-intoxicating cannabinoid found in cannabis, to help them quit smoking cigarettes as well as other drugs. At the same time, emerging research suggests that CBD indeed might be a novel treatment to treat addictions. However, the research itself is sparse and we do not have enough information from clinical trials to judge CBD as an effective medicine for treating addictions.
What is clear is that there is a dire need to improve treatments for addiction. Although some pharmacological treatments exist, e.g. varenicline for smoking, a majority fail to maintain long-term abstinence; therefore, it is necessary to invest in novel therapeutic drugs to improve treatment outcomes in addiction.
What is addiction?
Addiction is a chronic, relapsing brain disorder that is characterised by compulsive drug seeking and use. Several stages are involved in the cycle of addiction (see below), and one of the reasons that treatments for drug addictions are difficult is because not one medication can treat all of these stages. Addiction is characterised by continued drug taking despite negative consequences. Negative emotional states after withdrawal can trigger a relapse, which is one of the reasons why the cycle of addiction can have such negative outcomes on people’s lives. Relapse and craving after a period of withdrawal is a major target for pharmacotherapies for drug addiction.
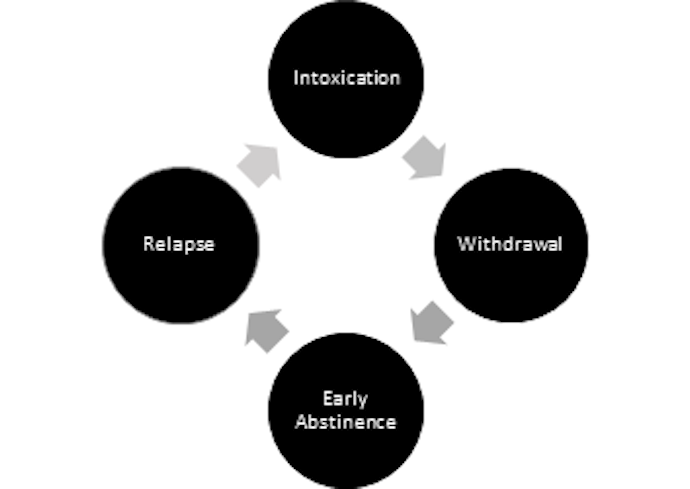
The cycle of addiction in several stages. Medications for the treatment of addiction can target any stage but no drug is yet a panacea for all stages. (Hurd et al. 2015)
What are the properties of CBD that might make it a useful drug for the treatment of addictions?
CBD is a cannabinoid found in cannabis, which has a broad profile of pharmacological actions that are still being debated. There is also an emerging literature on the antipsychotic properties of CBD but here we are going to concentrate on the properties that make CBD a potentially ideal candidate for cessation.
1. It’s not addictive – it has low reinforcing and low abuse
One of the properties that makes CBD a worthwhile drug to investigate for addictions is that it is not addictive. Unlike THC, the primary psychoactive cannabinoid found in cannabis, CBD is ‘placebo-like’ on all measures of abuse liability, including up to doses of 800mg. CBD does not change heart rate, blood pressure, body temperature or produce any intoxicating effects.
2. There are minimal side effects
CBD is safe in humans and animals up to doses of 1,500mg/day. Therefore, unlike current treatments for addictions that have side effects such as nausea and dry mouth, CBD can be taken without any unwanted symptoms.
3. Reduces anxiety
Anxiety is a key component of addiction. An important feature of CBD is that it reduces anxiety and negative emotional states implicated in addiction. As well as anxiety disorders and addictions being highly comorbid, anxiety is also a common symptom of withdrawal that can lead to relapse. CBD has been shown to be an effective anxiolytic; it reduces THC-induced anxiety, as well as the anxiety induced by simulated pubic speaking, even in people with an anxiety disorder. From a neuroimaging perspective, CBD reduces blood flow in areas associated with anxiety e.g. amygdala and hippocampus suggesting its use as a treatment for the anxiety associated with withdrawal is viable.
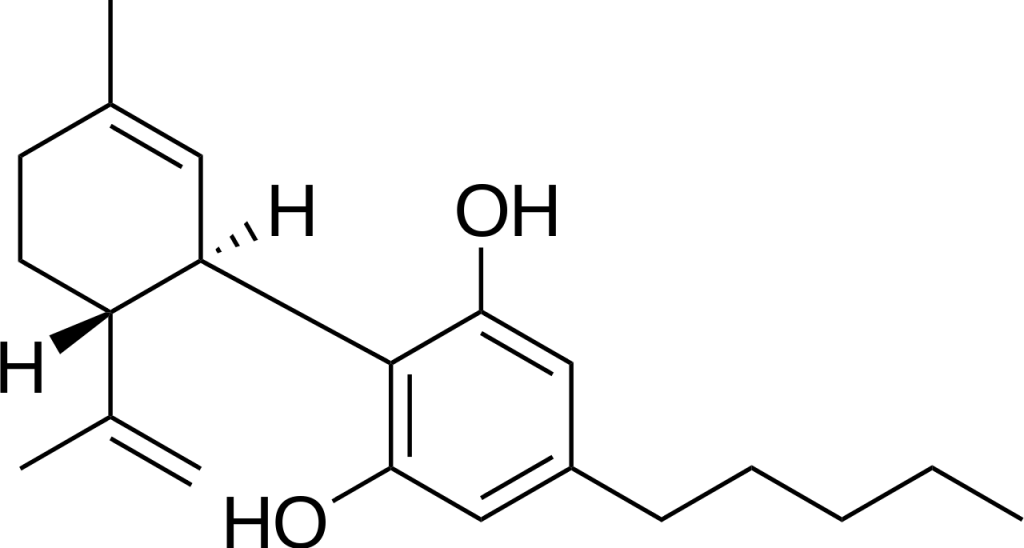
Cannabidiol (CBD)
4. Neuroprotective + pro-cognitive
In animal models, CBD is also noted to have neuroprotective, anti-inflammatory and immunomodulatory effects. Moreover, CBD has been shown to protect against THC-induced memory and emotional processing impairments.
Research with animals suggests that CBD can reduce the motivationally rewarding properties of drugs, reduce drug seeking, craving and withdrawal. However, there is a lack of human, experimental and clinical research investigating CBD in the various stages of addiction. One small scale clinical study of CBD for opiate addiction found results consistent with the animal research wherein CBD reduced heroin related cue-induced craving in those addicted to heroin. This reduction in craving lasted a week after administration moreover this effect was related to anxiety induced by the cues. Another pilot study from our lab showed that a CBD inhaler, used when daily cigarette smokers felt the urge to smoke, reduced the total number of cigarettes smoked during treatment by ~40% but there were no effect on craving or anxiety. Data from pilot studies should be taken with a pinch of salt but these initial human studies do serve as a starting point to investigate CBD in clinical studies.
Given the rapidly changing socio-political landscape surrounding cannabis and its constituents, research with CBD is now gaining momentum. Currently, there is an on-going clinical trial of CBD for cannabis addiction running at UCL funded by the Medical Research Council. This is important, as there are currently no pharmacological treatments for cannabis dependence. Sativex, the GW-produced cannabis extract, has also been investigated for the same purpose and in comparison to placebo, significantly reduces cannabis withdrawal symptoms. Given that withdrawal severity from cannabis and from nicotine are of similar magnitude, we are also investigating whether CBD can reduce tobacco withdrawal symptoms (and if you would like to take part, you can find more information here).
The recent increase in commercial sales has meant that the UK Medicine’s Health and Regularly Agency has classified CBD for medical use only (Dec, 2016). It is important to leverage the opportunity and continue to investigate CBD and other cannabis constituents as therapeutic interventions.
Chandni Hindocha is a Phd student at the Clinical Psychopharmacology Unit at UCL studying Mental Health.
